Intra uterine device (IUD)
-
The intra uterine device (IUD) is a long-acting, and reversible type of contraception.
-
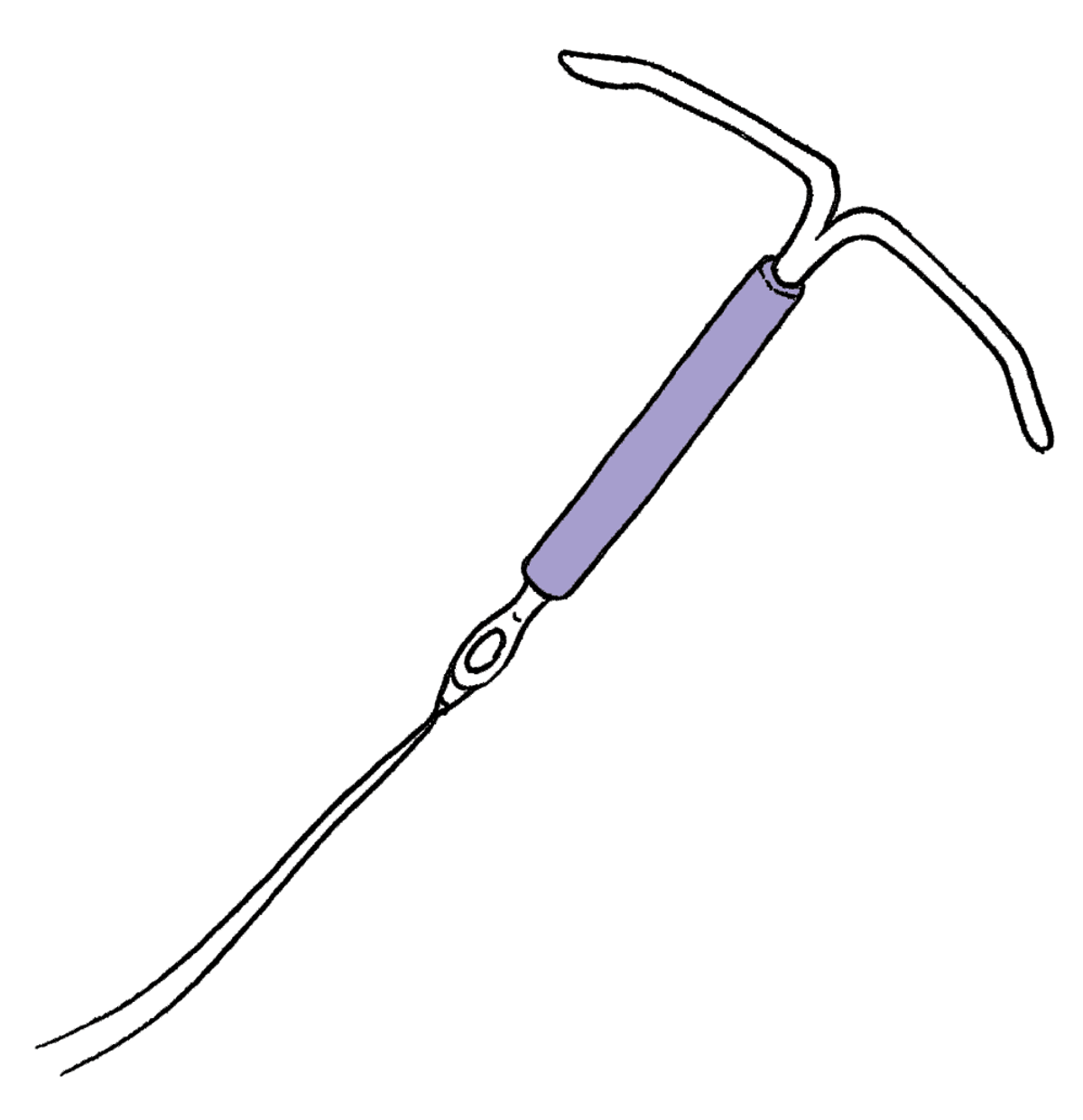
A hormonal IUD (not actual size)
-
Read this information in te reo Māori: Te taputapu roto kōpū (IUD)
The IUD is:
- Over 99% effective at preventing pregnancy
- Long acting — IUDs can work for 3-10 years depending on the type
- Fit and forget — you don't need to think about contraception every day
- Reversible — you can decide to have you IUD taken out at any time. After it's removed, your fertility will return to normal
- Breastfeeding friendly — IUD's have no effect on breastfeeding
The IUD isn't:
- Protection against sexually transmissible infections (STIs). — condoms and oral dams can protect against STIs
-
-
How do IUDs work?
-
An IUD is a small device that is put inside your uterus to prevent pregnancy.
The IUD is a long-acting reversible contraception (LARC). After you have your IUD put in, it can protect you from pregnancy for 3-10 years — or until you have it taken out.
There are two types of IUDs:
- The hormone IUD — this IUD uses progestogen to protect you from pregnancy
- The copper IUD — this IUD uses copper to protect you from pregnancy
Both types of IUD can stop sperm from getting to your egg. If your egg does receive a sperm, the IUD stops your egg from implanting in the wall of your uterus.
-
-
How well do IUDs work?
-
IUDs are more than 99% effective. That means less than 1 out of every 100 people who use an IUD will get pregnant every year.
-
-
How long do IUDs work for?
-
Your IUD can last for 3-5 years, depending on the type of IUD you choose to use.
You can decide to have your IUD taken out at any time.
You may be able to keep your IUD in longer if you are in your 40s. If you get a copper IUD put in after you turn 40 — or a hormone IUD put in after you turn 45 — your IUD may be able to stay in place until menopause. We can help you work out if this a good idea for you.
-
-
What are the advantages and disadvantages of an IUD?
-
Advantages:
- Can stay in place for 3 years or more
- Fit and forget
- You don’t need to think about contraception every day
- Doesn't affect breastfeeding
- Doesn't get in the way of sex
- The copper IUD doesn't contain any hormones
- The copper IUD can also be used as emergency contraception
- The hormonal IUD has a very small amount of hormones — most people have no side effects
- The hormonal IUD can help with period bleeding and pain — most people will have light bleeding or no periods at all
Disadvantages:
- Doesn’t protect against STIs
- Needs to be inserted or removed by an experienced doctor or nurse
- Copper IUDs may cause heavier periods or cramping
- Hormonal IUDs may cause irregular bleeding for the first few months
-
-
What are the side effects or risks of an IUD?
-
There is a small risk of infection — about 1% — when an IUD is put in.
There is a very small risk of damage to the uterus — about 1 in 1000 people. This risk is a bit higher, up to 6 in 1000 people, if you are breastfeeding.
If you get pregnant with an IUD in, there is a chance of pregnancy complications.
A copper IUD might give you more bleeding and cramping during your period — but this usually gets better over time.
The copper IUD can cause an allergic reaction. This is very rare.
The hormonal IUD might give you irregular or light bleeding — but this usually gets better over time.
The IUD can sometimes come out by itself — about 5% of all IUDs do this. We can teach you how to check the threads are still in the right place at any time.
-
-
Is the IUD painful?
-
Some people do find an IUD insertion painful, other people have light cramps, and some people feel no pain. Some people go home to rest for a few hours after getting an IUD, other people feel fine to get on with their day. Either way, it’s a good idea to take some pain killers before your appointment. When you make your appointment, you can ask us what painkillers to use, and how many to take.
You IUD will be put in by a trained professional. Don’t worry! They will take care of you, and will be able to answer any questions you might have.
-
-
What do you need to know about getting an IUD for the first time?
-
If you're not sure about the IUD, it’s a good idea to book an appointment to talk with us. We can help you work out what contraception types are best for you.
You can get your IUD put in any time that suits you — as long as you're not pregnant, or at risk of being pregnant.
Some good times to get an IUD put in are:
- While you have your period or just after you have your period
- Four weeks after you have a baby
- At the time of a surgical abortion
- As emergency contraception. You can use the copper IUD as emergency contraception for up to 5 days after unprotected sex. If you to, you can keep your IUD in after this — to use as long-acting contraception
Most of the time, you can get an IUD put in at your first appointment. If you can’t get an IUD put in at your first appointment, it might be because:
- We can’t be reasonably sure you’re not pregnant
- You haven’t had a period since taking emergency contraception (ECP)
- You have heavy bleeding which needs to be checked out
- It's difficult to insert the IUD
If you can’t get your IUD at your first appointment, we will usually work out when you can get it put in. We will make you another IUD appointment for that time.
-
-
How do you get an IUD?
-
How do you have your IUD removed?
-
Can you get an IUD for emergency contraception?
-
The copper IUD can be used as emergency contraception.
It can be put in up to 120 hours — five days — after unprotected sex, or within five days of your earliest expected date of ovulation.
If you have had unprotected sex and you want an IUD, book an appointment to talk with us. We can help you work out if it’s the best idea for you.
-
-
Can an IUD help you with heavy or painful periods?
-
The hormone IUD can help with heavy or painful periods.
Most people with a hormone IUD will have light bleeding or no periods at all. If you want a hormone IUD to help manage your bleeding, the nurse or doctor may want to check why you have heavy bleeding, before the IUD is put in.
If you have heavy or painful periods, you should not get a copper IUD because it might make your periods worse.
-
-
Does an IUD protect you from STIs?
-
IUDs don't protect you from sexually transmissible infections (STIs).
Condoms, oral dams, and regular STI testing are the best ways to protect yourself from STIs.
-
-
Can you get pregnant with your IUD in?
-
Pregnancy is very rare while using an IUD.
If you do get pregnant — or think you might be pregnant — while using an IUD, see your nurse or doctor as soon as possible. There is no extra risk to the developing embryo, but there is a risk of pregnancy complications.
If you want to continue the pregnancy, it’s best to get your IUD removed. This needs to be done early, to lower the risk of infection and miscarriage.
-
-
Can you get pregnant after your IUD is taken out?
-
You can get pregnant as soon as your IUD is taken out.
-
-
What is the Essure contraceptive device?
-
The Essure contraceptive device is different from other IUDs used in New Zealand, including copper and hormonal IUDs. It was used as permanent contraception, and is not reversible contraception like these other IUDs.
If you have had an IUD inserted at Sexual Wellbeing Aotearoa (formerly Family Planning New Zealand) you will not be using Essure. If you have any concerns about your contraception, please contact the health provider that inserted it.
-
-
How do you get an IUD?
-
An IUD must be put in — or taken out — by a trained medical professional. Our expert nurses and doctors can put in — or take out — your IUD. It’s an everyday procedure at our clinics, so you can trust us to take good care of you.
-
-
How we can help you
-
Our nurses and doctors are IUD experts. They can help you work out if the IUD is a good idea for you — and help you pick between the copper and hormone IUD.
We have experienced nurses and doctors who are trained to put in and remove IUDs.
Anyone can visit our clinics. If you want to talk with us, we want to talk to you.
-
-
-
Do you need urgent help?
If you require medical advice outside of our opening hours, call Healthline for free on 0800 611 116 anytime or get help from an after-hours medical centre or emergency services.